Long-term sickness: How worsening mental health is holding back the economy
Economic inactivity, driven by long-term sickness, is fast becoming one of the most pressing challenges facing the UK economy.


Economic inactivity, driven by long-term sickness, is fast becoming one of the most pressing challenges facing the UK economy.
2.7m people are out of work due to ill-health, up from 2.1m people pre-pandemic. The increase in long-term sickness means the UK is the only G7 economy where employment remains below its pre-pandemic level.
Clearly, worsening health is bad on an individual level, but it is fast becoming apparent that worsening health among the population is slowing growth and contributing to sticky inflationary pressures.
So what’s behind the problem and what is the government trying to do about it?

What’s behind the rise in long-term sickness?
One factor more than any other explains the recent rise in long-term sickness – deteriorating mental health.
ONS research from last July suggested that 53 per cent of those inactive due to long-term sickness had mental health conditions, although often as a secondary condition.
Mental health issues have been particularly prevalent among younger people (18-24). Young people are now more likely to experience a common mental disorder than any other age group, according to Resolution Foundation research.
Deteriorating mental health has contributed to a doubling in the number of young people out of work for health reasons in the past decade, jumping from 93,000 to 190,000.
“The proportion of young people out of work with mental health problems is rising pretty rapidly in a way that other health conditions aren’t,” Louise Murphy, senior economist, told City A.M.
There are other factors explaining the increase in long-term sickness, but worse mental health – particularly among young people – is a key part of the story.
Counting the cost
Its very difficult to quantify the cost of the recent increase in long-term sickness specifically, but the government is clearly having to spend a lot more to support a sicker population.
According to government estimates, spending to support disabled people and people with health conditions currently stands at £72bn, up from just under £50bn in 2003.
This is expected to rise by around £30bn in 2028/29, to £101bn. To put that into perspective, Hunt’s total 4p cut to National Insurance over the past couple of fiscal events cost £20bn.
Looking into what’s driving the increase in spending shows how deteriorating mental health is driving up government spending.
Take personal independence payments (PIP), a non-means tested benefit paid out to compensate for the costs associated with living with a disability. In 2019, there were an average of around 2,200 new PIP awards a month in England and Wales where the main condition was anxiety and depression – this has more than doubled to 5,300 a month last year.
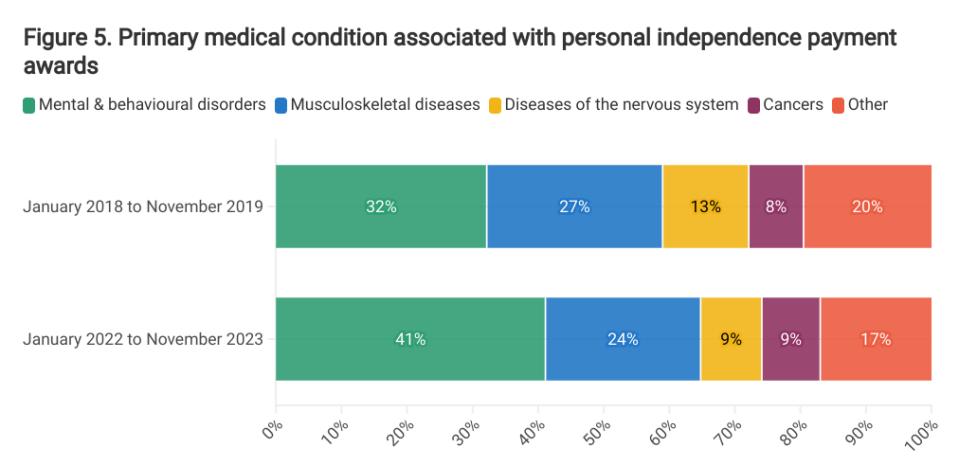
Just over 40 per cent of new PIP awards since the pandemic cited mental illness as the main factor, up from 32 per cent pre-pandemic. Again, research from the IFS shows that increases have been fastest in proportional terms among younger people.
The government estimates that PIP spending is expected to grow by 52 per cent from 2023/24 to £32.8bn by 2027/28, which it argues is “unsustainable”.
What is the government doing to tackle it?
The government’s approach to getting people back into work has been targeted at the role of mental health, both in words and in action.
Rishi Sunak has argued that everyday concerns are being “over-medicalised”, while Mel Stride, minister for Work and Pensions, has suggested that mental health culture has “gone too far”. Both have argued that, in many cases, getting people back into work can actually improve mental health.
The government’s approach is classic carrot and stick: try and provide better support for those who really need it while making it more difficult to receive welfare for those deemed unworthy. A tricky line to draw.
Last Autumn, it announced plans to expand four major programmes offering support to people with mental health conditions, including expanding access to NHS Talking Therapies by 384,00 places and Individual Placement and Support by 100,000 spaces.
In total, the expansion to the four programmes will lift participation by around 45,000, the OBR estimated.
These measures came alongside tightening eligibility criteria on other benefits and ramping up penalties for those who refused to look for work or take jobs which were offered.
The rhetoric was clearly more focused on the stick than the carrot. “If you are taking taxpayers for a ride – we will take your benefits away,” Stride said at the time.
This week, the government revealed plans for a major overhaul of PIP, which Stride argued would update the benefit to reflect the changing nature of disease. One proposed reform was to substitute cash payments for those with “milder” mental health problems with ‘tailored support.’
Will it work?
The big question hanging over the government’s approach is whether there’s been an objective deterioration in mental health or whether its all just snowflakery, for want of a better word.
If the former, it seems unlikely that changes to the welfare regime would do little to get people back into work, since it would not address the underlying issue.
Andy Bell, chief executive at the Centre for Mental Health, argued that there’s strong evidence “the nation’s mental health has been deteriorating over recent years”.
NHS data suggests that in 2023, just under 22 per cent of 20-25 year olds suffered from a ‘probable mental disorder’, up sharply from 16.6 per cent in 2021.
Similarly, analysis of 2021/22 data by the Royal College of Psychiatrists showed that referrals for secondary mental health service were up 26 per cent from 2018/19, to a record 4.6m.
Bell pointed to a range of factors, including the legacy of the pandemic and social media, but he also pointed to the “erosion” of youth services and social care as government support for these services has been cut.
Existing mental health support systems are already very stretched with nearly 2m people on waiting lists for mental health support.
“If the Government is serious about reducing the costs of social security, it needs to address the causes of poverty and disability,” he argued.
Murphy also argued that the government needed to focus its attention on prevention to stop the recent increase becoming a new trend.
“Historically, very few people who have been inactive for more than a couple of years return to work,” she said. “Prevention or early intervention is much more effective than trying to encourage people who have been economically inactive for a long periods of time to re-enter work,” she continued.
A government spokesperson said: “Our welfare reforms will help an extra one million people break down the barriers to work, as we shift the focus from what people can’t do to what they can”.


